Treatment in Germany is comprehensive. A blood test is part of the diagnosis.
A complete blood count is a basic test that is performed at the very initial stage of examining a patient.
The general blood picture includes:
To determine the immune status, an immunoglobulin test is used
Even minor changes in health affect the composition of the blood.
A general blood test helps a doctor of any specialty. Based on the results of a blood test (hemogram), the doctor can competently assess the condition of the body, make a preliminary diagnosis and promptly prescribe appropriate treatment.
So, a general (clinical) blood test shows:
● number of red blood cells,
● C-reactive protein
● hemoglobin content,
● number of leukocytes,
● leukocyte formula
General blood test indicators
An increase in the number of red blood cells is a sign of diseases such as leukemia, chronic lung diseases, and congenital heart defects.
Anemia (decreased number of red blood cells) can be caused by stress, increased physical activity, and fasting.
In humans, 1 mm³ of blood contains 4.5-5 million.
Low hemoglobin can be the result of large blood loss; a decrease in hemoglobin occurs when there is a lack of iron, a necessary material for the construction of hemoglobin. Also, low hemoglobin (anemia) is a consequence of blood diseases and many chronic diseases not associated with them.
A hemoglobin level higher than normal can be an indicator of many blood diseases, and a complete blood count will also show an increase in red blood cells. Increased hemoglobin is typical for people with congenital heart defects and pulmonary heart failure. An increase in hemoglobin can be caused by physiological reasons; after significant physical activity, the hemoglobin level may be higher than normal.
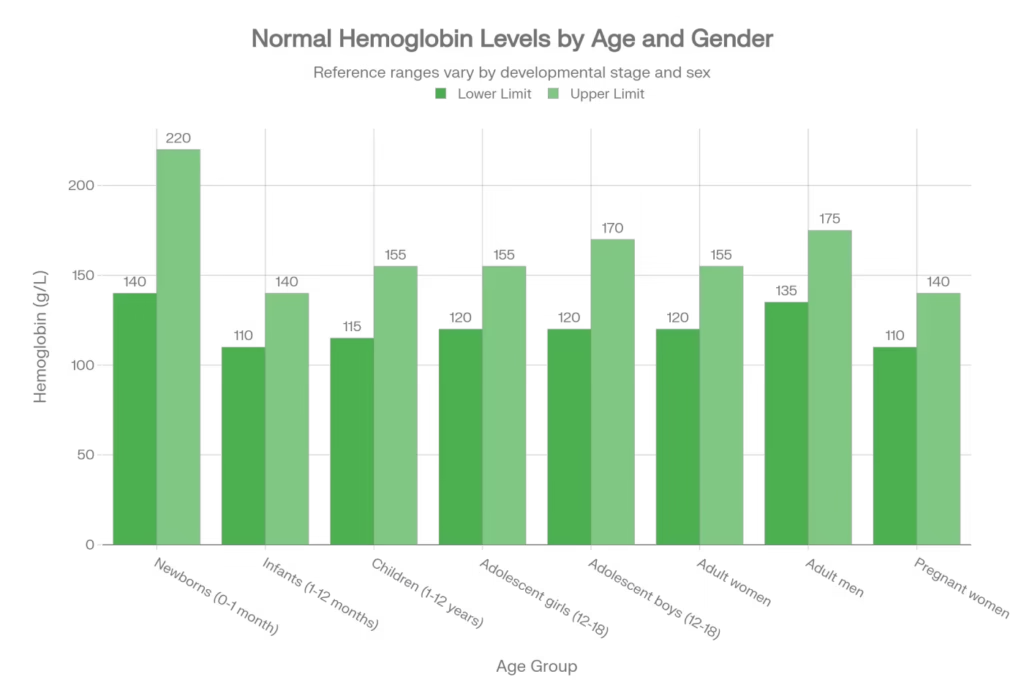
The normal content of hemoglobin in human blood is considered to be: for men 130-170 g/l, for women 120-150 g/l; in children – 120-140 g/l.
Hematocrit is the percentage (as a percentage) of the total blood volume that is made up of red blood cells. Normally, this figure is 40-48% for men, 36-42% for women.
The volume of erythrocytes compared to plasma increases with:
- dehydration (dehydration), which occurs with toxicosis, diarrhea, vomiting;
- congenital with heart defects, accompanied by insufficient oxygen supply to the tissues;
- a person being in high altitude conditions;
- insufficiency of the adrenal cortex.
The volume of red blood cells relative to plasma decreases with blood thinning (hydremia) or with anemia.
Leukocytes are the protectors of our body from foreign components. Leukocytes fight viruses and bacteria and cleanse the blood of dying cells.
There are 5 types of leukocytes:
- lymphocytes,
- monocytes,
- eosinophils,
- basophils;
any change in their ratio indicates various pathological changes in the body. For example, with elevated eosinophils it occurs with allergies, parasites, and malignant neoplasms. At birth and postoperatively, eosinophil levels are normal. Elevated monocytes are observed in leukemia, tuberculosis, and syphilis. Also, leukocytes in increased numbers mean the presence of viral, fungal or bacterial infections (pneumonia, tonsillitis, sepsis, meningitis, appendicitis, abscess, polyarthritis, pyelonephritis, peritonitis), and also be a sign of poisoning of the body. Burns and injuries, bleeding, myocardial infarction, lung, kidney or spleen, acute and chronic anemia, malignant tumors – all these “troubles” are accompanied by an increase in the number of blood leukocytes.
In women, a slight increase in leukocytes in the blood is also observed in the period before menstruation, in the second half of pregnancy and during childbirth.
A decrease in the number of white blood cells, which a blood test can show, may be evidence of viral and bacterial infections (influenza, typhoid fever, viral hepatitis, sepsis, measles, malaria, rubella, mumps, AIDS), rheumatoid arthritis, kidney failure, radiation sickness, some forms of leukemia, bone marrow diseases, anaphylactic shock, exhaustion, anemia. A decrease in the number of leukocytes can also be observed while taking certain medications (analgesics, anti-inflammatory drugs).
The blood of an adult contains an average of 4-9×10 9 leukocytes/l.
Platelets – these cells are also called blood plates. They are the smallest blood cells. The main role of platelets is participation in blood clotting processes. A decrease in the number of platelets is observed in women during menstruation and during normal pregnancy, and an increase occurs after physical activity. Typically, platelet control is prescribed when taking certain medications, when a person’s capillaries burst for no reason or nosebleeds are frequent.
An increase in the number of platelets in the blood (so-called thrombocytosis) occurs when:
- inflammatory processes (acute rheumatism, tuberculosis, ulcerative colitis);
- acute blood loss;
- hemolytic anemia (when red blood cells are destroyed);
- conditions after removal of the spleen;
- observed during treatment with corticosteroids;
- some rarer diseases.
A decrease in the number of platelets (thrombocytopenia) is observed in a number of hereditary diseases, but appears much more often in acquired diseases.
The number of platelets decreases when:
- severe iron deficiency anemia;
- some bacterial and viral infections;
- liver diseases;
- diseases of the thyroid gland;
- the use of a number of medications (vinblastine, chloramphenicol, sulfonamides, etc.);
- systemic lupus erythematosus.
C-reactive protein is a protein normally found in blood plasma. It is synthesized in the liver and is involved in immune defense. Its concentrations in the blood depend on the inflammatory response in the body.
The synthesis of C-reactive protein in the liver is stimulated by inflammatory molecules called cytokines.
Indications for CRP testing
C-reactive protein testing is justified in the following cases:
- If inflammatory, infectious and non-infectious diseases are suspected. Tissue damage. C-reactive protein testing is mainly used for: diagnosis, disease monitoring, treatment and prognosis.
- Diagnosis of intercurrent infections – surgery, toxic therapy, deep vein thrombosis, pulmonary embolism
- Diagnosis of anatomically closed infections
- Malignant processes
- Postoperative follow-up
- Acute coronary syndromes
- Risk of coronary artery disease, brain and peripheral vascular diseases (CRP-hs!)
Reference values for C-reactive protein
Control values are up to 5 mg/l. With inflammation, the amount increases many times over. Below we present the most common value changes by infectious agent type:
- Gram/-/CRP bacteria above 500 mg/l
- Gram/+/<50 mg/L (rarely below 100 mg/L)
- Parasitic infestations: slight increase in CRP concentration
- Viruses and mycoses: slight increase in CRP