В этой статье вы узнаете:
Bow-Leg Deformity (O-shaped legs, genu varum): diagnosis and treatment for adults in Germany
No waiting list for our patients
Bow-leg deformity is one of the most common orthopaedic conditions in adults. Even with the feet together, the knees remain apart and the legs take on a clear O-shape. In medical terms this is called genu varum.
In children, mild bowing often settles by itself. In adults it never corrects on its own. As the years go by, load on the joints increases, osteoarthritis develops, pain appears and movement becomes limited.
Unlike childhood bowing—usually a normal growth phase—adult bowing is acquired. The main driver is knee osteoarthritis: as cartilage wears on the inner (medial) side, load shifts inwards, the joint “sinks” medially and the leg axis moves into varus. So in adults, bowing is usually secondary to degeneration, not something you’re born with. That’s why it matters: if the axis isn’t corrected, arthritis progresses faster and the deformity worsens year on year.
We support adult patients who need modern minimally invasive treatment and rehabilitation in Germany.
Send us your X-rays and we’ll organise a free case review with a German orthopaedic surgeon.
Causes of bow-leg deformity in adults
- Childhood factors left untreated (Blount’s disease, rickets).
- Fractures and injuries with mal-union (bones healing in the wrong position).
- Chronic overload (excess weight, sport, heavy physical work).
- Inflammatory and degenerative disease (osteoarthritis, rheumatoid arthritis).
- A combination: congenital tendency + injury + weight → severe adult deformity.
In adults, varus deformity never self-corrects and tends to progress.
Symptoms and complications
- What you see: O-shaped legs; a gap between the knees with the feet together.
- Function: inner-knee pain, fatigue, crunching/clicking, stiffness.
- Complications: knee osteoarthritis, knock-on changes in hips and spine, joint contractures.
- Psychological impact: self-consciousness, reduced confidence and activity.
If you’ve persistent knee pain and visible bowing, book diagnostics with our specialists.
Adult diagnosis
Orthopaedic examination and gait assessment.
Full-length standing X-ray — the gold standard.
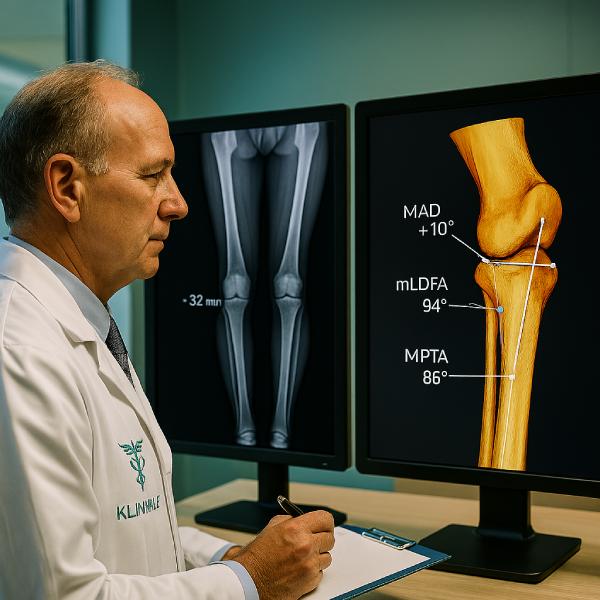
Measuring the mechanical axis (MAD) and angles HKA, mLDFA, MPTA.
CT/MRI for complex cases.
Modern 3D surgical planning.
Lab tests (vitamin D, calcium, bone density).
We refer patients only to clinics using digital imaging and 3D modelling, which reduces errors.
Conservative treatment in adults: what helps and what’s a myth
- Insoles & footwear: offload the joint but don’t correct the axis.
- Exercise therapy (physio): strengthens muscles but doesn’t change bone alignment.
- Physiotherapy: improves circulation, reduces swelling; doesn’t fix the deformity.
- Medication: eases pain; doesn’t correct the axis.
- Weight reduction: truly lowers joint load; doesn’t straighten the legs.
In adults, conservative care prepares you for surgery and slows complications but doesn’t remove the deformity.
Modern minimally invasive options & new technologies
Genicular Artery Embolisation (GAE)
GAE is a minimally invasive procedure increasingly used in Germany. Through a tiny puncture in the thigh artery, a catheter is guided to small vessels feeding inflamed knee tissues. Microparticles partially block abnormal blood flow, reducing inflammation.
Benefits:
- less pain,
- reduced swelling,
- improved mobility,
- can delay bigger surgery by several years.
Best for:
- adults with varus + osteoarthritis,
- those unfit for osteotomy,
- anyone who needs to buy time.
GAE doesn’t straighten the leg, but helps you stay active and prepare for surgery.
Exo-Muscle & supportive devices
Prototype exoskeletons (Exo-Muscle) unload the joint while walking. Useful for:
- early osteoarthritis,
- the rehabilitation phase,
- patients not yet ready for surgery.
Combined “trio-therapy”
A combination of insoles, braces and physiotherapy performs better than any single measure.
Ask us whether GAE or supportive devices are suitable in your case as a temporary solution.

Surgical treatment for adults
Open-Wedge Osteotomy
Bone is cut, the wedge is opened to the planned angle and fixed with a TomoFix plate. Very precise; healing can be a bit slower.
Closed-Wedge Osteotomy
A bone wedge is removed and the bone is realigned and fixed. Heals faster; less flexibility for fine adjustment.
Hexapod systems
External fixators enabling gradual correction; used for complex deformities.
Minimally invasive techniques
Small incisions 3–5 cm, modern plates (LCP, TomoFix), robot-assisted navigation (MAKO, Brainlab) with accuracy to about 1°.
We partner with clinics where these technologies are standard.
Send your scans and we’ll match you with a minimally invasive surgeon.
Post-operative rehabilitation in Germany
- Days 2–3: up with crutches.
- Weeks 2–3: partial weight, hydrotherapy pool.
- Weeks 6–8: full weight bearing.
- Months 3–6: low-impact sport.
- Months 6–9: full sport/activity.
Methods: Lokomat robotic gait trainers, pool-based therapy, physiotherapy, massage, cryotherapy, psychological support.
We reserve places in German rehab centres for 3–6 weeks of intensive therapy.
Get your personal rehab plan from us before surgery.
Outcomes & results
- pain reduced or gone,
- better gait and cosmetic appearance,
- slower arthritis progression,
- long-term effect 10+ years,
- return to sport.
We prepare a full package — diagnostics, surgery, rehab, interpreter and logistics.
Contact us to receive a tailored cost estimate within 48 hours.
Frequently Asked Questions (FAQ)
What is bow-leg deformity and what are the symptoms?
Genu varum (O-shaped legs) means the knees curve outwards. Standing with feet together leaves a visible gap between the knees. Key adult symptoms: visible bowing, pain in knees/feet/hips (worse with activity), uneven shoe wear (outer edge), altered gait, easy fatigue, a sense of knee instability.
Why does it occur in adults?
Residual childhood issues (e.g., rickets), injuries with mal-union, knee osteoarthritis (especially medial), metabolic bone disease (e.g., Paget’s), and excess weight.
Can it be corrected without surgery?
Not fully. Physio, insoles, massage and conservative care reduce pain and slow progression, but don’t straighten bone. Best for early stages or combined with other treatments.
What happens if I ignore it?
Faster arthritis, chronic pain, gait and posture problems (including hips/spine), and reduced quality of life.
Do I have to have surgery?
Not always. It depends on deformity, symptoms and other conditions. Osteotomy (axis correction) or joint replacement may be advised if conservative care fails and pain or progression is significant.
Osteotomy vs knee replacement — what’s the difference?
Osteotomy realigns your own bone to offload the damaged part of the knee — often better for younger, active patients with localised arthritis.
Replacement swaps the joint for a prosthesis — used when arthritis is advanced and the joint is destroyed.
When can I return to work?
Desk work typically 2–3 weeks after surgery (if pain is controlled). Physical jobs: 3–6 months, once fully recovered and cleared by your surgeon.
Will there be scars?
Modern techniques keep scars small. Osteotomy or replacement may leave longer scars, but surgeons aim for thin, neat lines. After GAE, only a few tiny puncture marks that fade with time.
How long is rehabilitation?
After osteotomy: 6–12 months to full recovery (crutches for 6–8 weeks, then gradual loading).
After replacement: 3–6 months; walking from day one is common.
Is treatment suitable if I’m over 60?
Yes — age alone isn’t a contraindication. The decision depends on overall health, arthritis stage and goals. Older patients more often go for replacement.
When can I exercise?
Low-impact (swimming, cycling, walking) 3–6 months post-op. High-impact (running, jumping, field sports) 6–12 months, and only with medical clearance.
How long does surgery take?
Osteotomy 60–90 minutes, replacement 90–120 minutes, GAE 30–60 minutes.
Is treatment in Germany covered by Irish or EU insurance?
Yes. Under EU law (the EHIC and the Cross-Border Healthcare Directive), Irish patients are entitled to receive planned treatment in Germany with costs covered by the HSE. This means that for medically necessary operations such as osteotomy or joint replacement, your German hospital bills can be reimbursed by your Irish health insurance, provided the referral and approval process is followed.
Why Germany?
Highly trained surgeons, state-of-the-art technology, and structured rehabilitation embedded in care pathways.
Bow-leg deformity in adults isn’t just cosmetic — it’s a major driver of arthritis and chronic pain. German clinics provide a complete pathway: precise diagnostics, minimally invasive surgery, GAE as a supportive option, and mandatory rehabilitation.
We guide you from the first tests to full recovery, with clear pricing and support in English. We work only with leading orthopaedic centres recognised internationally.
Fill out the form on our site for a free consultation. Within 48 hours you’ll know which treatments suit you and the likely cost in Germany.
- NAME OF SERVICE ADDITIONALLYPRICE, €
- Diagnostics Diagnostics 550 €
- Osteotomy, including hospital stay of up to 7 days Orthopedic surgery from 18 000 €
- GAE Minimally Invasive Orthopedics 6000 €